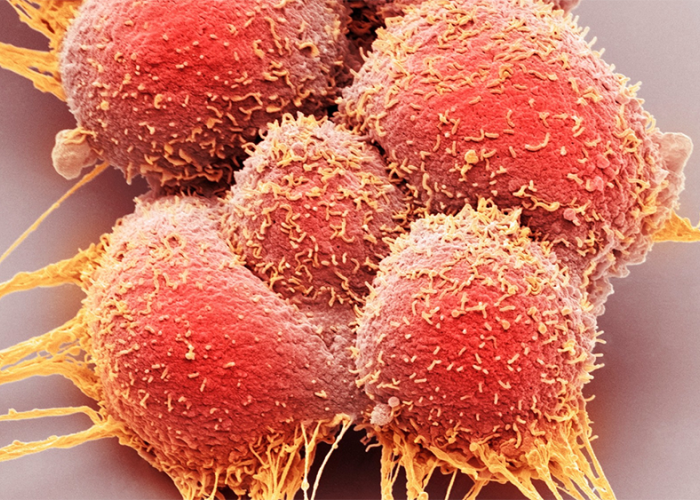
Characterised by additional aggressive cancer lesions in other parts of the body, the condition is found in around five to 10 per cent of prostate cancer patients at the time they are first diagnosed.
 An important new study led by BC Cancer scientist Dr. Alexander Wyatt is the first to indicate that cancer complexity within the prostate may be driving tumour proliferation in this patient population more than previously understood. Published in the journal Nature Cancer, this finding paves the way for new inroads in the development of precision treatments for de novo metastatic prostate cancer, as well as other aggressive cancers.
An important new study led by BC Cancer scientist Dr. Alexander Wyatt is the first to indicate that cancer complexity within the prostate may be driving tumour proliferation in this patient population more than previously understood. Published in the journal Nature Cancer, this finding paves the way for new inroads in the development of precision treatments for de novo metastatic prostate cancer, as well as other aggressive cancers.
“Because the danger from the spread of tumours in de novo metastatic prostate cancer is so pressing, treatment has often been directed more to targeting the metastatic cancer throughout the body than on the origins of the cancer within the prostate,” notes Dr. Wyatt, an associate professor in the department of urologic sciences at the University of British Columbia and Vancouver Coastal Health Research Institute researcher a senior research scientist with the Vancouver Prostate Centre and with BC Cancer. “However, we found that the diverse pool of cancer cells found within the prostate could be associated with multiple waves of cancer spread throughout the body, along with sources of treatment resistance.”
"This discovery indicates that there could be a biological and clinical rationale to remove or ablate the prostate to limit further spread of metastatic disease.”
Using the analogy of a tree, Dr. Wyatt explains the original prostate cancer can be thought of as the tree trunk. Cancers that spread from the prostate to other areas of the body — such as the lymph nodes, bones and lungs — are its branches. So long as the trunk exists, the tree can continue to produce new branches. However, destroy the trunk, i.e., through the removal or destruction of the prostate itself, and a primary cancer driver could be cut off.
Collaboration supported groundbreaking prostate cancer research findings
A key to Dr. Wyatt’s research findings was having rare access to a pool of over 600 biological samples from 43 patients diagnosed with de novo metastatic prostate cancer. In collaboration with a team of Belgian researchers led by Dr. Piet Ost, Dr. Wyatt and his team at the Vancouver Prostate Centre were able to analyze the whole prostates, along with pelvic lymph nodes and blood samples, of patients from a Belgian study.
Due to the severity of the disease, de novo metastatic prostate cancer patients often do not undergo surgery to remove the prostate, but instead immediately receive hormone therapy and sometimes radiation to treat the presence of tumours throughout the body. However, the Belgian study involved the removal of the whole prostate and pelvic lymph nodes prior to subsequent treatments, giving Dr. Wyatt’s team a glimpse of these tissues soon after diagnosis.
Access to the whole prostate was a crucial piece of the puzzle to understanding the development and spread of the disease. Dr. Wyatt and his team discovered that biopsies of several different regions were required to see the full breadth of cancer variation within a single prostate, as different areas contained divergent cancer mutations.
“One of the unique aspects of our study is that colleagues in Belgium made available to us a rare library of tissue and blood samples from de novo metastatic prostate cancer patients," noted Dr. Wyatt.
Thanks to these tissue and blood samples, Dr. Wyatt and his team developed a roadmap of the spreading branches of cancer from the prostate.
“While we developed this roadmap for prostate cancer, it may well have applications in other forms of cancer,” he said.
“We expect these findings will heighten the attention given to cancer variation as a driver of metastatic prostate cancer,” added Dr. Wyatt. “In addition, it is anticipated that downstream changes to clinical best practices may include the collection and analysis of additional prostate biopsies from each patient to better inform treatment decision-making.”
“These insights will help to further advances in the development of individualized prostate cancer care.”
The team is now applying their roadmap to study blood and tissue samples from approximately 500 de novo metastatic prostate cancer patients in British Columbia. With access to two to eight biopsy cores from the prostate of each patient, the team will have greater than average biological source material to study cancer mutations and heterogeneity.